Praedictio mortis conturbat me
Q: Did you see scientists have found a way to predict immediate death?
A: What? Lack of pulse?
Q: Very droll. No, it says interleukin-6. What is that?
A: It’s a messenger protein that some white blood cells use to stimulate other white blood cells to do stuff. If there’s a lot of it around, there’s probably inflammation, which is probably bad.
Q: And it’s new?
A: No.
Q: The story says it’s new.
A: Yes. Yes, it does.
Q: So what’s new?
A: Interleukin 6 and another marker of inflammation called C-reactive protein used to be thought of as the best things to measure if you cared about inflammation. Some researchers came up with another, called α1-acid glycoprotein, and said it was better. This research is arguing that, no, α1-acid glycoprotein isn’t better.
Q: Why isn’t α1-acid glycoprotein mentioned in the story?
A: It is: the Herald’s just having font problems and calling it α1-acid glycoprotein.
Q: Are they right? Is interleukin 6 really better than α1-acid glycoprotein?
A: We can’t really tell just from this one study, any more than we could really tell α1-acid glycoprotein was better from the study that liked it.
Q: How accurate is the prediction?
A: Well, suppose you were given the name of a 55-year old and had to guess whether they’d die in the next five years. What would you guess?
Q: Umm. No?
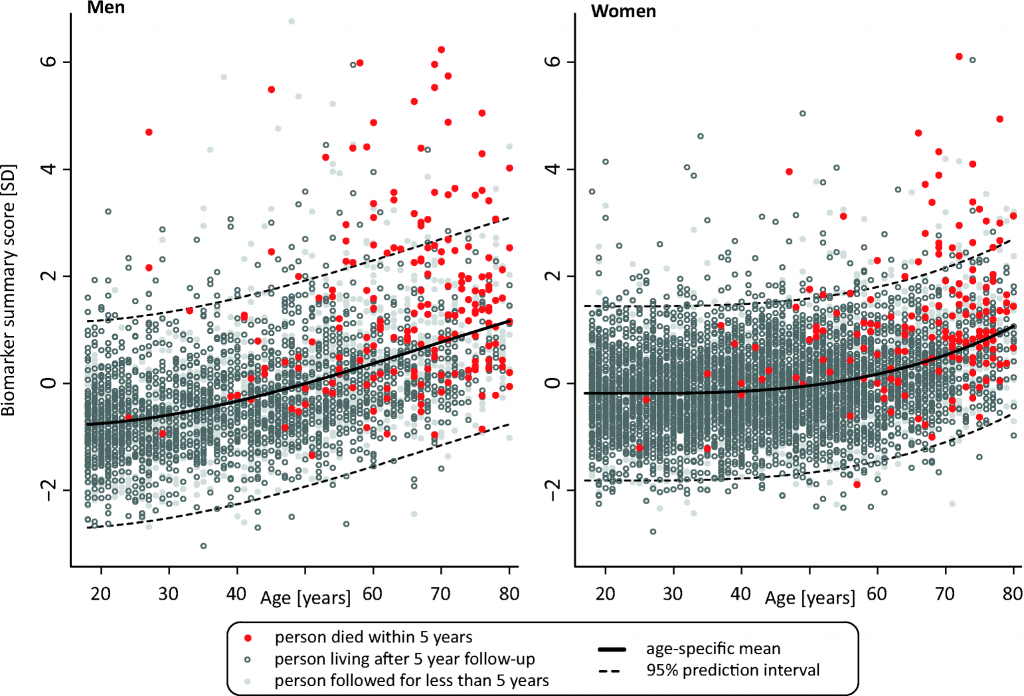
A: Very good. In this study, over 98% of the people didn’t die in the first five years of followup, so you’d be about 98% accurate knowing nothing.
Q: And knowing their interleukin 6 levels?
A: About 98% accurate.
Q: So it’s useless?
A: No, not at all. Comparing people at the top and bottom of the middle 50% of the distribution for interleukin-6 was like comparing smokers to non-smokers for short-term death rate. It’s just that will you/won’t you die in five years is not the right question for reasonably healthy middle-aged people.
Q: So it could be important for insurance, then?
A: In principle, if you wanted to undermine the usefulness of insurance. It’s more useful for science — either understanding how inflammation has its effects, or trying to rule it out as an explanation of a correlation.